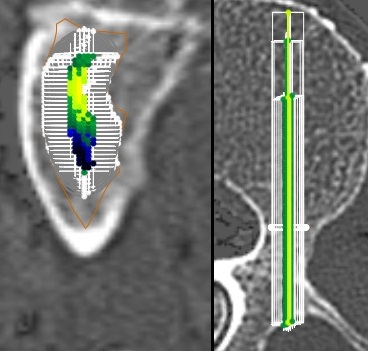
In green is what we would give for 100% of the patients as a first procedure: 78% will have a satisfactity clinical outcome.
But 22% of the osteopenic/osteoporotic patients will suffer from BMD related complication with this limited montage.
In blue and yellow: vertebral extention required for the 22% to avoid BMD related complication. Yellow indicates selective pedicle augmentation.
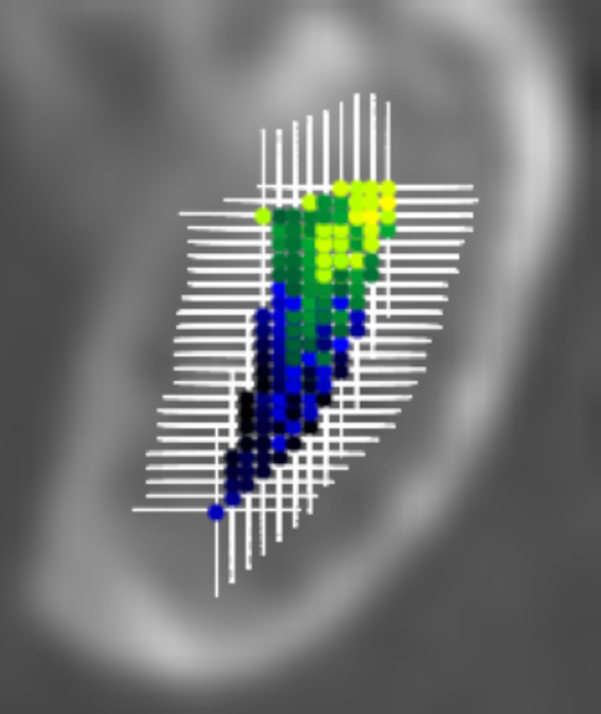

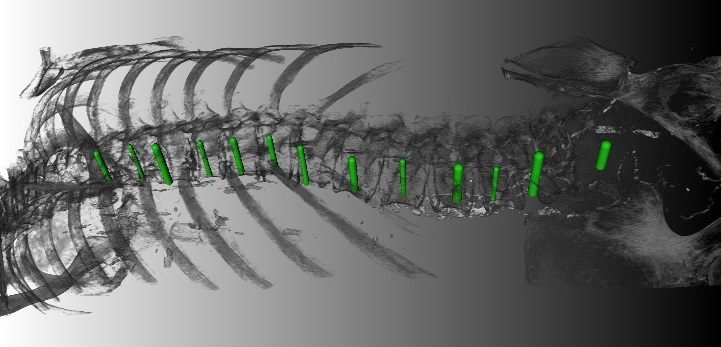
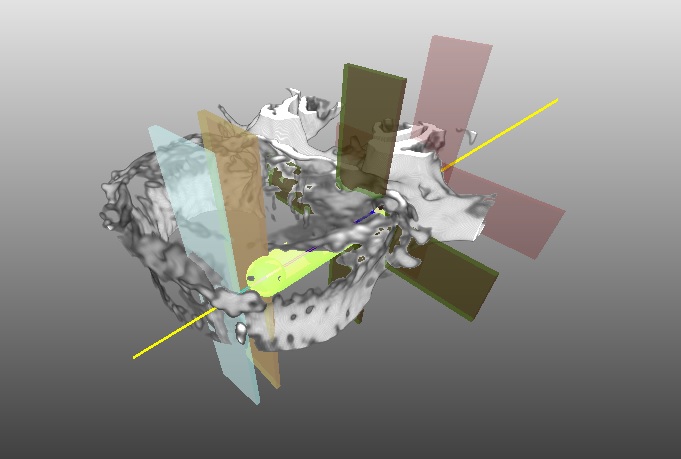
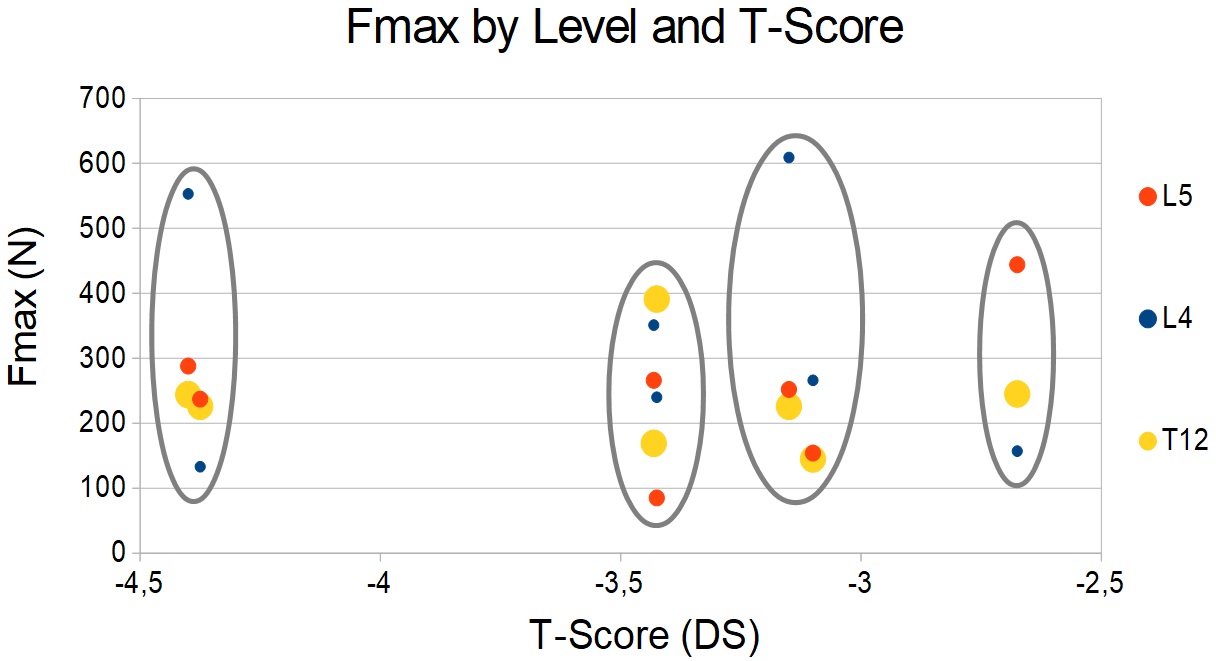


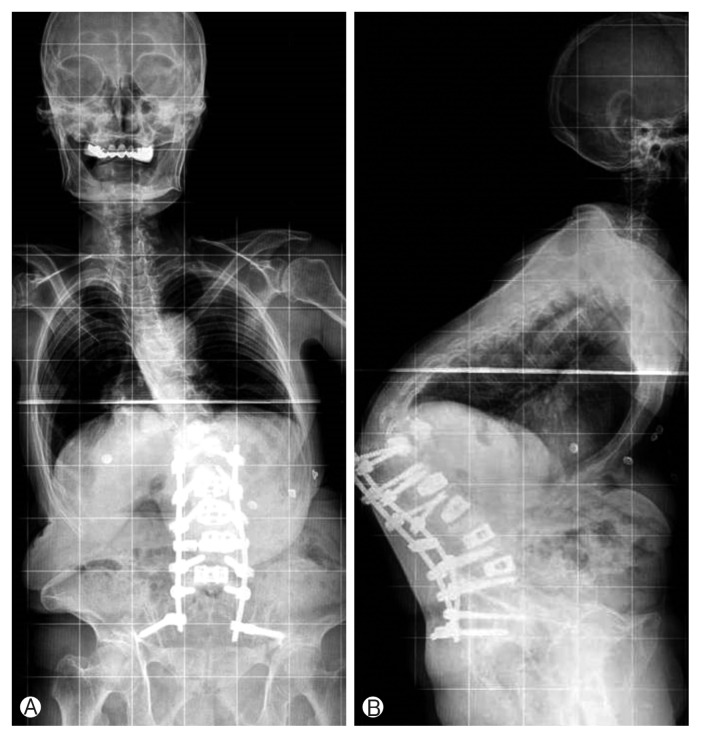
 ...and not necessarily all of this.
...and not necessarily all of this.